A Roadmap for More Equitable, Human-Centered Healthcare Research
0 min read
In decades past, individuals accessing health care were often relegated to a passive role in their own treatment. It was taken for granted that experts, like doctors and policymakers, knew what was best for their patients and the public.
Now, things are starting to change. While clinical and policymaking expertise remain an important aspect of health care, there’s a growing recognition of the importance of lay expertise, also known as lived and living experience. Simply put, people who have directly experienced some facet of the healthcare system have a uniquely meaningful perspective on it — one that should be treated as a crucial input to policy and treatment decisions. As the classic slogan goes: “Nothing about us without us.”
Engaging people with lived or living experience (PWLEs) in healthcare research has been shown to lead to better patient outcomes, as well as improve cost-effectiveness. It’s especially critical for addressing inequities in health care: people from marginalized groups face more barriers to accessing critical health care, and are at risk of poorer outcomes. In order to close these gaps, healthcare policy needs to be designed based on a nuanced understanding of the patient experience, which only PWLE can provide.
A definitive guide for health researchers
But not all PWLE engagement is created equal. Co-design is more complicated than sitting down for a one-off conversation, or sending a survey. Engagers need to be mindful about who they’re engaging and how. They also need to take steps to minimize risks — like the risk of retraumatizing research participants.
In reality, these best practices are not always realized when researchers reach out to PWLEs for co-design. Although there’s a growing ecosystem of informal resources to help researchers work with PWLEs ethically and effectively, the onus is on individual researchers to seek out and make sense of this information.
We partnered with Health Canada to address the gaps between PWLE engagement best practices and the reality on the ground. We worked with leading public health experts from Canada and beyond to distill this sprawling body of research on PWLE engagement into a centralized, evidence-based framework.
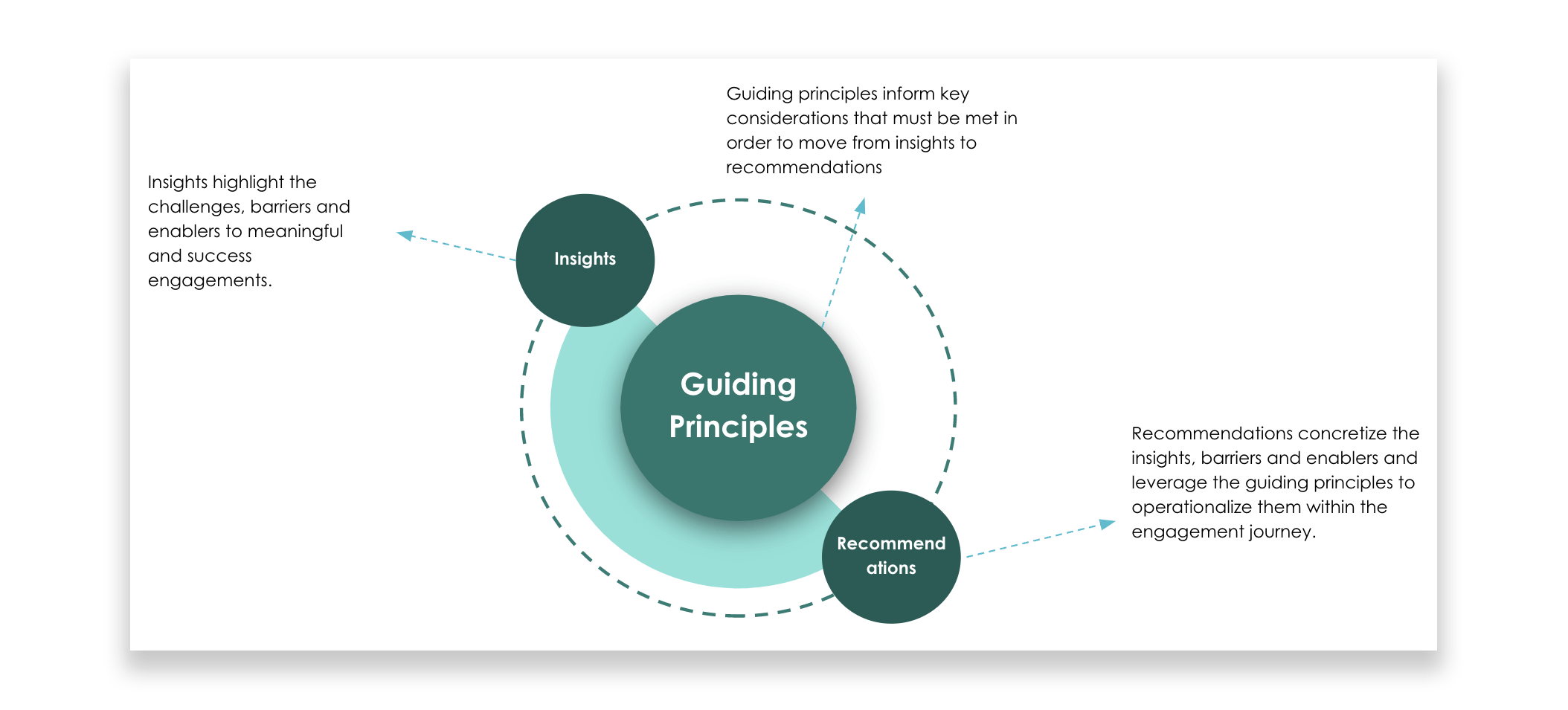
The result is a simple, actionable set of guiding principles that PWLE engagers everywhere can use in their work. We also identified key barriers and enablers to acting on these principles, then tapped into our expertise in behavioral change techniques (BCTs) and human-centered design to develop more than 30 tactical recommendations for addressing them.
Falling through the cracks
We all interpret the world through the lens of our own experiences. That means we all have blind spots: questions we’d never even think to ask if left to our own devices, and dimensions to the problem at hand that are completely invisible to us.
In health care, for example, policymakers have historically looked to patient outcome metrics as the most important indicators of how well the system is working. But this approach completely leaves out the issue of access: many groups, including low-income people and people of color, are less likely to seek out treatment in the first place. PWLE input is crucial for pointing out biases like this, and orienting decision-makers towards weaknesses in the system that they might never have thought about otherwise.
Empowering patient voices
At TDL, we have extensive experience co-designing healthcare solutions with marginalized groups. In our work on Wellness Together Canada, we recruited a research pool of more than 2,500 people from across Canada to help us design a groundbreaking digital mental health app.
The guidelines we developed for Health Canada were informed by our own past work. But the main inputs came from leading experts in this space: practitioners, researchers, PWLE advocates, and community organizers. We worked closely with them to identify the behavioral and structural obstacles to effective PWLE engagements. We also conducted a comprehensive review of the published literature on PWLE engagement and healthcare co-design.
Based on all of this information, we were able to map out the unique decision journeys that engagers undertake when they reach out to PWLEs, and identify the key touchpoints where they often run into behavioral and structural barriers. Our 30+ design recommendations use human-centered design principles to help researchers bypass those barriers.
We developed our design recommendations with the goals of making PWLE engagements both meaningful and successful for all parties involved. Co-design shouldn’t just be about extracting useful information from PWLEs; it’s an opportunity for engagers to forge enduring relationships with their research participants, and to empower them in sharing their experiences for the benefit of their communities.
Sometimes, simple changes to a research protocol — like sending the occasional update email to let PWLEs know how their contribution is helping — can make the biggest difference. When participants feel respected, supported, and encouraged by engagers, everyone benefits: it lowers the risk of harm for PWLEs, while also making them more likely to stick around for future research initiatives.
The road to healthcare equity
Our guidelines and recommendations are just one part of a major push by Health Canada to improve healthcare equity across the country. The guidelines and recommendations we developed are now helping to charter federally funded research, and to ensure that patients from all backgrounds have a voice in their own care.



















